
Pinnacle at GP24
This year marks a significant milestone for the Royal New Zealand College of General Practitioners (RNZCGP). To commemorate its 50th anniversary, the College’s annual conference, GP24, adopted the whakatauki, “kia whakatōmuri te haere whakamua – walking backwards into the future with eyes fixed on the past". The Hon. Dr Shane Reti, Minister of Health delivered a keynote speech; read the transcript here.
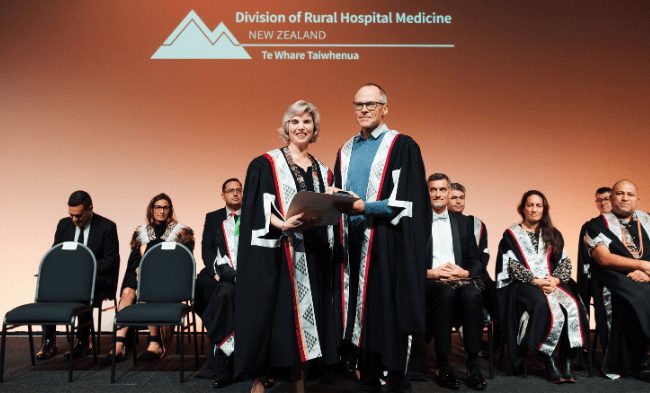
Distinguished Fellowship of the RNZCGP: Dr David Maplesden
Congratulations to Dr Dave Maplesden, who was among seven RNZCGP members to receive a Distinguished Fellowship. Dave has been a GP liaison since 2013 for Pinnacle Midlands Health Network and spent 12 years in the role of the College’s chief examiner for the GPEP1 written examination, passing on the baton in 2019.
Alongside Dr Jo Scott-Jones, Pinnacle’s clinical director, Dave speaks on The New Zealand General Practice podcast on a variety of GP topics – ranging from medical conditions, experiences from the frontline and sharing perspectives.
Dave is also passionate about quality, and for over 15 years has been serving as a medical advisor to the Health and Disability Commission (HDC) where he imparts calm and sensible advice on how to maintain our professional standards.
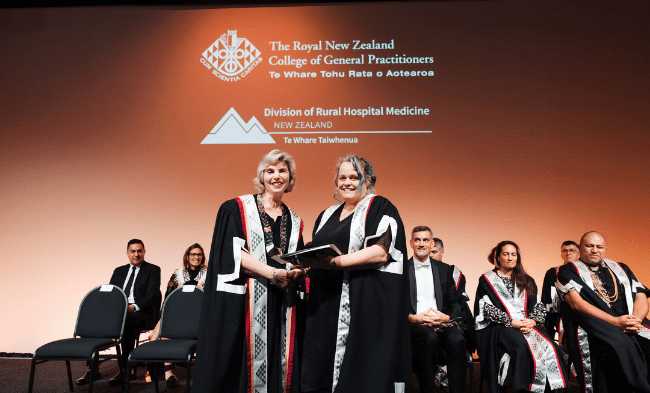
Eric Elder Medal: Dr Hayley Scott
Dr Hayley Scott (Health Ngātea) is this year's recipient of the Eric Elder Medal. This medal is awarded in honour of Dr Eric Elder, who was an inspirational rural GP affectionately known as the grandfather of vocational training in Aotearoa New Zealand. Hayley's nomination describes her as a doctor whose leadership at Pinnacle has contributed to the development of the Health Care Home and whose leadership of her team has led to expansion of the services provided to their community, expansion of their clinic from Te Aroha into Ngātea, and the creation of sustainable services through implementing health care home and taking on extended team members. She is also an inspirational teacher of undergraduates and registrars.
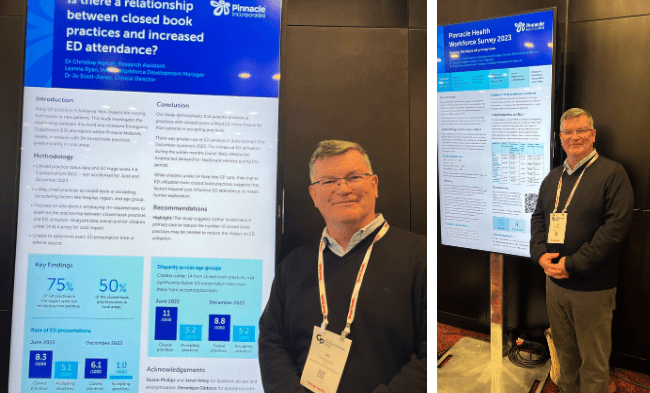
Pinnacle presentations
Pinnacle was a prominent contributor to the GP24 conference, with our team presenting sessions and e-posters, and others associated with Pinnacle participating in panel discussions. Here are some of the highlights from our network.
- Establishing a stable infrastructure for delivering POCT in general practice – experience from the Cyclone Recovery funded project (presentation).
Dr Jo Scott-Jones. - Reflections from the Pinnacle Extended Care Team: how we evolved to gather and intertwine whānau voice within service delivery (presentation).
Hannah Milner, Pen Blackmore. - Is there a relationship between closed book practices and increased ED attendance (poster).
Dr Christine Mercer, Research Assistant; Leanne Ryan, Health Workforce Development Manager; Dr Jo Scott-Jones, Clinical Director (presenter).
See our resource page for Pinnacle’s workforce survey reports. - Pinnacle Midlands Health Network General Practice workforce survey 2023 (poster).
Leanne Ryan, Health Workforce Development Manager, Dr Veronique Gibbons, Senior Project Manager, Dr Janet Amey, Senior Project Manager (presented by Dr Jo Scott-Jones). - Joint presentation: A primary care pathway to achieve general registration. Challenging the traditional roles of hospital-based attachments: the experiences of the Waikato NZREX General practice pilot programme 2023-2024.
Dr Joseph Scott-Jones (Pinnacle), Dr Wayne De Beer (Waikato Hospital).
Panel discussions
Rural Health - The challenges of today are the opportunities for tomorrow
Dr Fiona Bolden, Rural GP and Chair of Hauora Taiwhenua Rural Health Network, and Dr Alex McLeod, GP Coromandel Family Health Centre, joined the panel for this discussion on urgent action needed by rural health to address today’s challenges, and future opportunities. This discussion looked at innovative solutions and future directions for rural health in New Zealand.
How to future proof patients’ health, our practices and primary care from the effects of climate change
Dr Kiyomi Kitagawa, GP Carefirst practice, Taranaki, and Pinnacle Incorporated executive committee deputy chair, joined the panel for this discussion. Carefirst Taranaki has appointed a climate champion and implemented solar panels in one building, with funding from the Pinnacle facility fund. Kiyomi said the initiatives are expected to impact waste management. Additionally, the organisation is shifting prescribing practices from MDI to DPI and exploring social prescribing, including the development of a community garden. Carefirst Taranaki is working towards Toi Tu Carbon certification and ultimately, net zero emissions.
Extra reading: Climate action in practice (page 11, GP Voice June 2024)
Additional reference: One Health represents a recognition of the intimate link between human health, environmental health, and animal health.

Dr Jo Scott-Jones shares his thoughts on the workforce crisis, likening it to the perceived impossibility of the Chernobyl disaster.
Read moreThe Royal New Zealand College of General Practitioners supports research and education that benefits general practice, rural general practice and rural hospital medicine through three funding rounds each year. Applications for the final funding round of 2024 are now open.
Read moreThis new programme is a collaboration between Te Runanga o Kirikiriroa (Facilitation Service) and general practices.
View detailsGPs in each of our districts get frustrated when they hit barriers when seeking interventions from other providers. There is a perception that DHB services are becoming more difficult to access and that different DHBs have different levels of service available to their communities. This page outlines our process for advocating alongside practices.